Biology runs on timing. That’s the simple idea behind a new Health Affairs Branded Post by Paritosh Kaul, MD, and Wendy L. Wright, DNP, which examines proposed changes to the adolescent meningococcal vaccination schedule through the twin lenses of “natural laws” and patient-centered outcomes. Beneath the logistics of doses and acronyms, the authors argue, is a biological clock that doesn’t pause while policy catches up—and when we mistime protection, patients bear the risk.
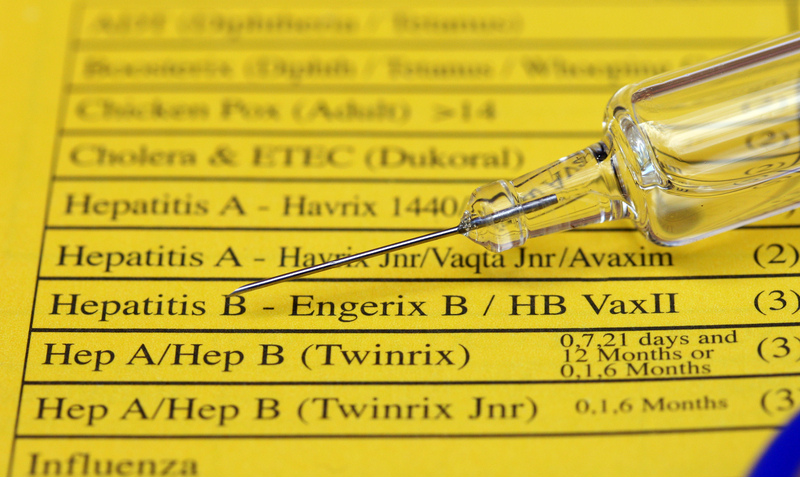
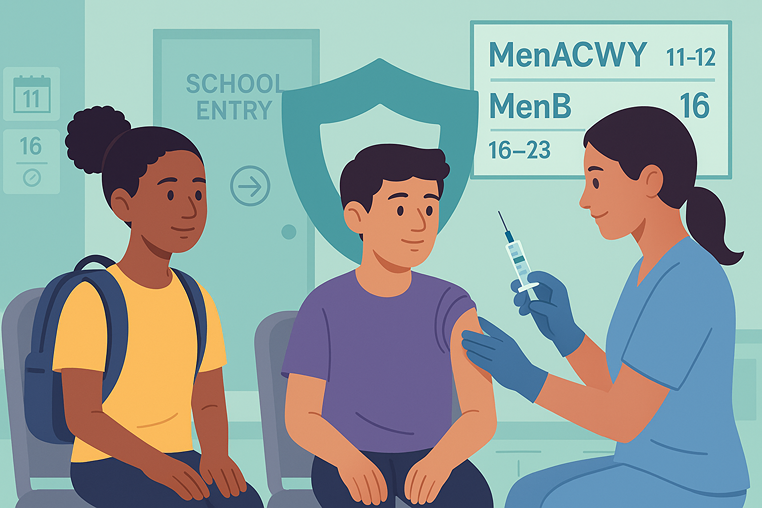
Today’s framework is intentionally staged to match immune development and real-world exposure. Adolescents receive the quadrivalent meningococcal ACWY vaccine (MenACWY) at ages 11–12, followed by a booster at 16. A separate meningococcal B vaccine (MenB) is recommended from ages 16 to 23, preferably at 16–18. This two-touch approach isn’t just convenient; it delivers early protection before the high-contact teen years and then reinforces it precisely when social mixing and risk rise. That cadence has helped drive adolescent meningococcal disease down.
The current policy discussion centers on a new pentavalent option, MenABCWY, and whether ACIP should simplify to a single dose at age 16. On paper, a one-and-done schedule promises administrative ease. In practice, the authors warn, it would create a protection gap from ages 11 to 16—exactly when exposure increases. Through a “natural laws” lens, delaying protection introduces avoidable windows of susceptibility. Biology isn’t a back-office process that can be deferred without consequence; it is the main stage, and timing missteps can show up as real cases and preventable harm.
Equity raises the stakes further. National coverage for MenACWY hovers around the high 80s, but not all adolescents are protected equally. The post highlights persistent shortfalls for Black and Hispanic teens relative to White peers, with even larger gaps when a second dose or booster is required. Those coverage differences intersect with higher disease and complication burdens in some minority communities, compounding vulnerability. In other words, if we remove earlier protection, the communities already facing lower coverage and higher risk could be hit hardest—and policy optimized for simplicity may underperform where the need is greatest.
There is also a practical backbone we can’t ignore: school-entry requirements. Dozens of states and Washington, D.C., currently rely on ACIP guidance to set middle-school MenACWY requirements, and research shows state policies tend to follow those federal recommendations with a multi-year lag. If ACIP drops the 11–12 recommendation, those middle-school requirements could unravel, weakening a proven delivery channel that raises vaccination rates and narrows disparities. The downstream effect isn’t theoretical; it would be felt in clinics, schools, and families deciding whether and when a teen gets protected.
What would a patient-centered update look like? The authors suggest ACIP broaden its recommendations beyond schedule mechanics to address delivery where gaps persist. That means targeted outreach in communities with lower coverage, integration of vaccination with routine care and school-based services, community-led access through trusted local venues, consistent equity surveillance with demographic reporting, and provider training that tackles implicit bias and vaccine-hesitancy conversations head-on. If policy changes proceed, pairing them with concrete steps that make access easier—especially for those who face the steepest barriers—can keep effectiveness, not just efficiency, at the center.
From the FYH.News perspective, three takeaways stand out. First, timing matters: the 11–12 plus 16 cadence reflects how immunity develops and how risk rises during adolescence. Second, equity matters: simplifying administration cannot come at the cost of widening gaps for the very populations who already see higher disease burden and more frequent complications. Third, delivery matters: if we change the schedule, we should invest in the systems that actually get shots to arms—school requirements, integrated care, and community pathways that meet families where they are.
Efficiency is valuable, but effective protection is non-negotiable. Any update to adolescent meningitis prevention should preserve early protection, reinforce the critical 16-year booster moment, and double down on access strategies proven to work in communities with the most barriers. That is how policy aligns with biology—and how systems reduce, rather than redistribute, patient risk.
Read the full analysis in Health Affairs to dig into the evidence and policy details, and join the conversation about aligning vaccination timing, delivery, and equity with the biological realities families face.
Read the Health Affairs Branded Post → Link
Join the discussion and learn more → Link
Trending Topics
Features
- Drive Toolkit
Download and distribute powerful vaccination QI resources for your community.
- Health Champions
Sign up now to support health equity and sustainable health outcomes in your community.
- Cancer Early Detection
MCED tests use a simple blood draw to screen for many kinds of cancer at once.
- PR
FYHN is a bridge connecting health information providers to BIPOC communities in a trusted environment.
- Medicare
Discover an honest look at our Medicare system.
- Alliance for Representative Clinical Trials
ARC was launched to create a network of community clinicians to diversify and bring clinical trials to communities of color and other communities that have been underrepresented.
- Reducing Patient Risk
The single most important purpose of our healthcare system is to reduce patient risk for an acute event.
- Jessica Wilson
- Subash Kafle
- Jessica Wilson