- By Victor Mejia

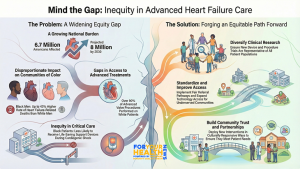
A new comprehensive review of interventional heart failure care warns that rapid advancements in treatment may be outpacing the nation’s ability to ensure equitable access. The paper examines persistent disparities across devices, procedures, and outcomes for patients with heart failure, concluding that communities of color, women, rural patients, and individuals with lower socioeconomic status continue to face disproportionate barriers to lifesaving care.
Heart failure affects nearly 6.7 million people in the United States, a number expected to reach 8 million by 2030 according to the American Heart Association. For communities of color, the burden is even heavier. A 2019 study published in the Journal of the American College of Cardiology found that Black men had up to a 43 percent higher rate of heart failure–related cardiovascular deaths than White men, with similar trends among Black women. Researchers attribute these disparities to a combination of structural racism, socioeconomic conditions, environmental risks, and uneven access to specialty care.
The new review underscores how these systemic inequities shape the landscape of interventional heart failure, a field that includes remote monitoring technologies, transcatheter valve procedures, revascularization, and advanced mechanical circulatory support. While such interventions can improve survival and quality of life, the authors find that many of the benefits are not reaching patients who need them most. They note that clinical trials supporting device approvals often lack representation from Black, Latino, Indigenous, and Asian populations, as well as from women—raising concerns about whether findings can be generalized to the broader population. In studies of remote cardiac monitoring, for example, women represented as little as 2 percent of participants, despite experiencing high rates of heart failure with preserved ejection fraction.
The review also details inequities in the real-world use of these technologies. Remote monitoring devices have been shown to reduce hospitalizations by detecting early signs of worsening heart failure, yet they are less commonly offered to women and people of color. Cost and insurance coverage remain major barriers, particularly for low-income and rural patients. The authors note that these devices are often used more frequently in large teaching hospitals than in community settings, leaving entire regions with fewer opportunities to access early-intervention tools that could prevent complications.
Disparities in Advanced Procedures Raise Alarms
Transcatheter valve interventions—such as transcatheter aortic valve replacement and mitral transcatheter edge-to-edge repair—represent some of the most significant innovations in heart failure treatment. However, the review shows that racial and ethnic minorities remain dramatically underrepresented in the clinical trials that established these procedures. Real-world data reflect similar disparities. Registry analyses indicate that more than 90 percent of valve procedures in the United States are performed on White patients, even though Black and Latino patients face comparable or higher levels of disease burden. In follow-up studies, minority patients who did receive procedures were more likely to be hospitalized for heart failure within a year, which researchers believe may reflect delayed diagnosis or inconsistent referral pathways.
The review identifies similar concerns in the area of coronary revascularization. Major trials evaluating percutaneous coronary intervention often excluded patients with severe heart failure and included very small numbers of Black and Hispanic participants. In a pooled analysis of more than 22,000 patients undergoing coronary stent procedures, Black and Hispanic participants had higher rates of adverse cardiovascular events even when presenting with less severe disease. The findings raise questions about whether guideline-directed care fully reflects the needs of populations facing the greatest risks.
Cardiogenic shock—the most severe form of heart failure—reveals the starkest disparities. Mechanical circulatory support devices such as intra-aortic balloon pumps and Impella pumps improve survival for patients in shock, but multiple studies show that Black patients are less likely than White patients to receive these devices. Among women, rates of device utilization are also lower, and complication rates higher. A national analysis of extracorporeal membrane oxygenation found that while mortality improved for White patients over time, outcomes for Black and Hispanic patients remained unchanged.
Experts in cardiovascular equity say those patterns reflect longstanding weaknesses in the health care system, from referral bias to geographic maldistribution of specialized cardiac centers. Dr. Clyde Yancy, a cardiologist and national leader in health equity, has written that disparities in advanced heart failure care represent the “avoidable consequences of structural inequity,” warning that without major system-wide changes, innovations will continue to benefit only a subset of the population.
The authors of the new review emphasize that addressing these inequities will require action across clinical care, research, and policy. They call for greater diversity in clinical trials, improved technology access for low-income and rural communities, standardized referral pathways, and the use of implementation science to identify and eliminate bias in treatment decisions. They also highlight the importance of community partnerships to build trust and ensure that new interventions are designed and deployed in culturally responsive ways.
As heart failure rates climb nationwide, the review offers a clear warning: technological innovation alone will not close the widening gaps in outcomes. For communities of color and other groups disproportionately affected by heart failure, equitable access to new devices and procedures may determine whether survival improves or disparities deepen. The authors argue that the future of interventional heart failure must be shaped not only by scientific advancement but by a commitment to ensuring that all patients can benefit from it.
Stay Informed. Stay Empowered.
Also Read: Proposed NIH Cuts Threaten U.S. Biopharma Leadership, Experts Warn
Trending Topics
Features
- Drive Toolkit
Download and distribute powerful vaccination QI resources for your community.
- Health Champions
Sign up now to support health equity and sustainable health outcomes in your community.
- Cancer Early Detection
MCED tests use a simple blood draw to screen for many kinds of cancer at once.
- PR
FYHN is a bridge connecting health information providers to BIPOC communities in a trusted environment.
- Medicare
Discover an honest look at our Medicare system.
- Alliance for Representative Clinical Trials
ARC was launched to create a network of community clinicians to diversify and bring clinical trials to communities of color and other communities that have been underrepresented.
- Reducing Patient Risk
The single most important purpose of our healthcare system is to reduce patient risk for an acute event.
- Subash Kafle
- Subash Kafle
- Jessica Wilson