Maternal mental health has become a quiet emergency for Black and Brown mothers in the United States. National groups estimate that about 1 in 5 new mothers experience a maternal mental health condition such as depression or anxiety. A fact sheet from the Maternal Mental Health Leadership Alliance says almost 40% of Black mothers will experience a maternal mental health condition – almost twice the rate of all women. Many never receive treatment or even a formal diagnosis, even though recent data show that mental health conditions, including suicide and overdose, are now among the leading causes of death during pregnancy and in the year after birth, according to national maternal mortality reports and advocacy groups.
For women of color, the risks are layered. A recent report from the Connecticut Health Foundation found that Black mothers in that state experience life-threatening pregnancy complications at twice the rate of white mothers, and that women of color make up most maternal suicides in Connecticut. Nationally, a 2020 “Vital Signs” report from the Centers for Disease Control and Prevention (CDC) found that about 1 in 8 women with a recent live birth reported postpartum depressive symptoms, and many said they were never asked about depression by a health-care provider during prenatal or postpartum visits. A 2023 CDC study in the journal Preventing Chronic Disease reported that 7.2% of women had depressive symptoms 9 to 10 months after giving birth, and more than half of them had not reported symptoms earlier in the postpartum period. That means depression can appear late, after most routine follow-up has already ended. These numbers show why maternal mental health must be treated as a core part of maternity care, not an optional extra.
These numbers are not just statistics. Advocates say they reflect daily realities for mothers who are trying to recover from childbirth, feed their babies, return to work, and keep their families stable while struggling with sadness, fear, or emotional numbness. March of Dimes describes maternal mental health conditions as “one of the most common complications during pregnancy and the postpartum period” and warns that too many women never receive care. Advocates say that fixing maternal mental health for Black and Brown mothers will require long-term investment in community-based care, not just short-term projects.
Across racial and ethnic groups, experts now use the term “perinatal depression” for depression that starts during pregnancy or within a year after delivery. Research suggests that race and racism strongly influence who develops these conditions and who gets help. A recent study in JAMA Network Open reported that Black mothers have the highest prevalence of postpartum depression among racial and ethnic groups studied, underscoring how social stress, discrimination, and unequal access to care shape mental health during and after pregnancy.
Gaps in Care for Black and Brown Mothers
Studies have found that women from racial and ethnic minority groups are less likely to be screened for postpartum depression in the first place. Researchers at the Massachusetts General Hospital Center for Women’s Mental Health and others have reported lower screening rates for African American, Asian, and other non-white women compared with white women, especially among younger mothers, those covered by Medicaid, and people who are not fluent in English. When depression is not picked up early, mothers may continue to suffer in silence, and symptoms can become more severe.
Stay Informed. Stay Empowered.
At the same time, Black women are more likely to experience maternal mental health conditions but less likely to receive care. A fact sheet from the Maternal Mental Health Leadership Alliance says that almost 40% of Black mothers will experience a maternal mental health condition, and that Black women are about twice as likely as white women to face these conditions yet only half as likely to get treatment. Other national summaries of research suggest similar patterns for Hispanic and Indigenous mothers: perinatal mood and anxiety disorders are a leading underlying cause of pregnancy-related deaths for Hispanic birthing people, and postpartum depression rates among American Indian and Alaska Native parents are estimated to be between 14% and 30%.
Advocates and researchers stress that these gaps are not about individual choices, but about systems. Organizations such as Black Mamas Matter Alliance describe Black maternal health as more than just physical care. They argue that true care also means protecting Black women’s peace, boundaries, and full humanity in medical settings and in their communities. Long-term exposure to racism, financial stress, unsafe housing, and unstable work can raise the risk of depression and anxiety during and after pregnancy. These same structural problems can make it harder to attend appointments, find child care, or afford therapy.
Stigma is another barrier. Some Black women describe feeling pressure to be the “strong” one in their family or community and worry that sharing mental health struggles will lead to judgment or even involvement from child protective services. Maternal mental health advocates say fear of being labeled an “unfit mother” can make it harder for women to be honest about intrusive thoughts, trauma, or exhaustion, especially with providers who do not share their background or understand these fears.
Experts also point to how the health-care system is organized. In many places, standard postpartum care still centers on a single check-up around six weeks after birth. A recent national poll from a “State of Maternal Health” report found that about two-thirds of respondents said they had postpartum mental health struggles, yet more than half felt unsupported by their providers, and many said one visit was not enough. Because mental health symptoms may appear before, well after, or between scheduled visits, especially for parents juggling work, child care, and physical recovery from birth, short-term follow-up can leave serious conditions undetected.
Some medical groups are calling for stronger action. The American College of Obstetricians and Gynecologists (ACOG) has issued guidance urging clinicians to identify and eliminate racial and ethnic inequities in obstetric and gynecologic care, including maternal mental health. In a 2024 March of Dimes statement, Kelly Ernst, the group’s chief impact officer, warned that “too many moms are experiencing mental health conditions” and said that people facing racial or economic inequities are more likely to be affected, underscoring the need for better screening and support.
On the ground, cities and community groups are testing new models. In Brownsville, Brooklyn – a neighborhood with some of the highest maternal mortality rates in New York City – the city Health Department recently launched a “Neighborhood Stress-Free Zone,” a pilot program that offers free massages, mental health screenings, parent classes, perinatal yoga, and help with social needs for pregnant and postpartum people. Local coverage and city health officials say the program aims to lower maternal deaths, especially among Black women, by combining clinical care with emotional and practical support and by making services easier to reach in the neighborhood. Community-based doulas, midwives, and peer support groups in Black and Latino neighborhoods around the country play a similar role, though access often depends on local funding, insurance coverage, and workforce shortages.
National advocates say policy changes are also needed. The federal Black Maternal Health “Momnibus” package, for example, would expand Medicaid coverage for postpartum care, invest in community-based organizations, and improve data on maternal mental health and mortality among Black, Latino, and Indigenous families. Public health agencies and nonprofits also promote tools like the national Maternal Mental Health Hotline (1-833-TLC-MAMA), which offers free, confidential support by phone or text in English and Spanish and can connect families with local resources.
Advocates say that closing postpartum support gaps for Black and Brown mothers will take more than one new program or an awareness campaign. They argue that care must be redesigned so mental health screening is universal and ongoing, providers are trained to recognize bias and listen to mothers’ concerns, and community-based services are funded at the same level as hospital care. As Black Mamas Matter Alliance and other groups often point out, true maternal health equity will only be reached when every mother has the rights, respect, and resources to feel safe, heard, and supported in the months after birth – not just to survive childbirth, but to heal and thrive.
Also read: reporting on Black maternal health inequities from the Connecticut Health Foundation and CT Insider; the CDC’s 2023 study on the timing of postpartum depressive symptoms; and local coverage of New York City’s Neighborhood Stress-Free Zone pilot in Brownsville for pregnant and postpartum families.
For more on how NMQF is supporting women of color during pregnancy and after birth, see NMQF’s story on the Lift Every Voice HerHealth Hub
Trending Topics
Features
- Drive Toolkit
Download and distribute powerful vaccination QI resources for your community.
- Health Champions
Sign up now to support health equity and sustainable health outcomes in your community.
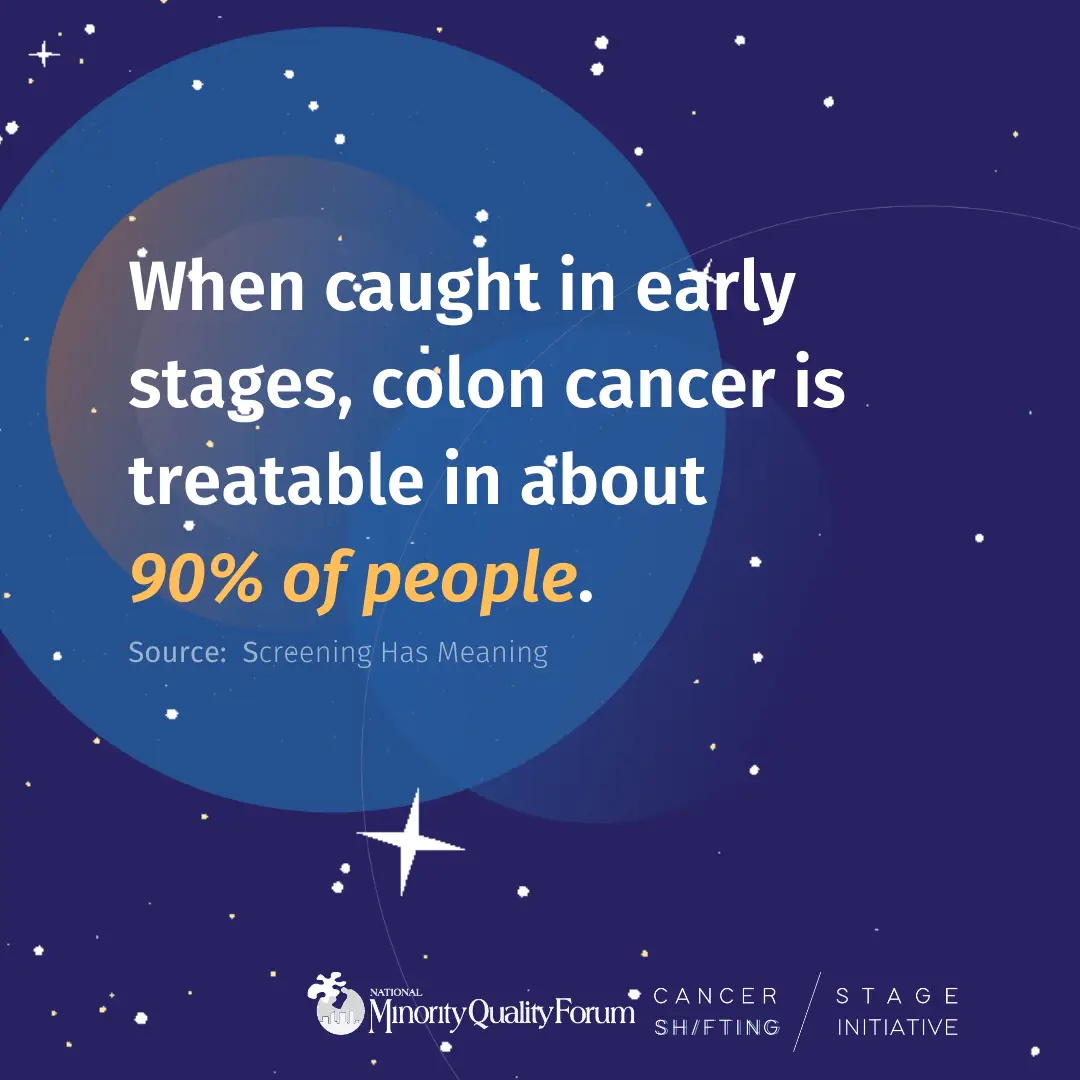
- Cancer Early Detection
MCED tests use a simple blood draw to screen for many kinds of cancer at once.
- PR
FYHN is a bridge connecting health information providers to BIPOC communities in a trusted environment.
- Medicare
Discover an honest look at our Medicare system.
- Alliance for Representative Clinical Trials
ARC was launched to create a network of community clinicians to diversify and bring clinical trials to communities of color and other communities that have been underrepresented.
- Reducing Patient Risk
The single most important purpose of our healthcare system is to reduce patient risk for an acute event.
- Jessica Wilson
- Victor Mejia
- Subash Kafle