Cancer continues to exact a disproportionate toll on Black Americans decades after the civil rights era reshaped the nation’s social landscape, medical experts say, underscoring enduring inequities in health care that trace back to structural racism and unequal access to quality treatment. A new report from the American Cancer Society shows Black people in the United States are still more likely than other racial and ethnic groups to die from many common cancers, even as overall cancer death rates have fallen in recent years. According to the latest data, cancer mortality among Black men and women declined significantly between 1991 and 2022 — by nearly half for men and one-third for women — but continues to outpace deaths among White and other populations. In 2025, researchers estimate there will be roughly 248,470 new cancer diagnoses and 73,240 cancer deaths among Black people in the United States, with cancer remaining the second-leading cause of death after heart disease in this population.
Public health officials and clinicians point to these persistent disparities as a reflection of long-standing barriers that many Black Americans face in the health system. “This report highlights the disparities the Black community has faced for decades,” said Dr. Wayne A. I. Frederick, interim chief executive officer of the American Cancer Society. He noted that while the declines in mortality rates are encouraging, stark inequities in incidence and survival for many cancers “underscore the urgent need for targeted research and interventions.”
Data from the American Cancer Society and federal health agencies reveal marked differences in outcomes for specific cancers. Black men are more than twice as likely as White men to die from prostate cancer, and Black women are about 40 percent more likely to die from breast cancer than White women, despite slightly lower incidence in some age groups. Across most cancer types and stages, survival rates for Black patients lag behind those of their White counterparts.
Experts attribute these gaps to a complex interplay of social determinants of health — including socioeconomic factors, access to preventive services, and the quality of care received — that disproportionately affect communities of color. A joint analysis by the National Cancer Institute showed that while cancer death rates among Black individuals have declined over time, they remain higher than those of other racial and ethnic groups. Researchers noted that delayed diagnosis, limited access to timely treatment, and poorer quality of care are likely contributors to these disparities. “Black individuals continue to have a delay in care or receive poorer care than their White counterparts,” said a lead investigator in that study.
Historical context is crucial to understanding these patterns. Black Americans have long faced systemic obstacles in accessing health care, from segregated hospitals before the 1960s to persistent economic inequalities today. These structural factors can affect everything from early detection — such as routine cancer screenings — to the prompt initiation of treatment and follow-up care. Studies have shown that discrimination at provider visits and lower rates of high-quality screening contribute to later-stage diagnoses and reduced survival.
Community health leaders emphasize the role of outreach and culturally competent care in addressing disparities. Screening for cancers like colorectal and breast, timely access to advanced therapies, and patient education around symptoms and risk factors are all seen as essential components in narrowing the survival gap. At the same time, researchers are calling for a broader focus on policies that address income inequality, neighborhood resources, and other social drivers that influence health outcomes.
Public health advocates also stress the importance of representation and trust in the medical system. Patients who feel understood and respected by providers are more likely to seek preventive services and adhere to treatment plans. “Expanding access to high-quality cancer prevention, early detection, and treatment for all Americans” is critical, one American Cancer Society expert said, noting that improved health equity requires systemic change beyond the clinic walls.
Despite the challenges, there have been improvements. The overall decline in cancer mortality among Black Americans reflects progress in reducing smoking rates, improvements in treatment, and earlier detection for some cancers. These advances illustrate how public health interventions and medical innovation can save lives, but they also highlight how unevenly the benefits have been distributed across racial and ethnic groups.
Efforts to close these gaps are increasingly linked to broader conversations about racial justice and health equity in the United States. Organizations serving Black communities are advocating for research that explicitly examines and addresses the effects of structural racism on health outcomes, as well as tailored interventions that can reach underserved populations more effectively.
As the nation observes occasions such as World Cancer Day and Black History Month, health professionals and community leaders stress the urgency of sustaining momentum in cancer prevention and care. They argue that acknowledging the historical and social roots of health disparities is a necessary step toward eliminating them. Closing the cancer mortality gap will require concerted effort from policymakers, health systems, researchers, and communities alike to ensure that advances in cancer care benefit everyone equitably.
In the final analysis, the ongoing disparities in cancer outcomes among Black Americans stand as a stark reminder that progress in medicine must go hand in hand with progress in social equity. The path forward, experts say, lies in bridging gaps in access and quality, strengthening community-based initiatives, and fostering a health care environment where race no longer predicts outcomes.
Also Watch: Flint Forward Live
Stay Informed. Stay Empowered.
Trending Topics
Features
- Drive Toolkit
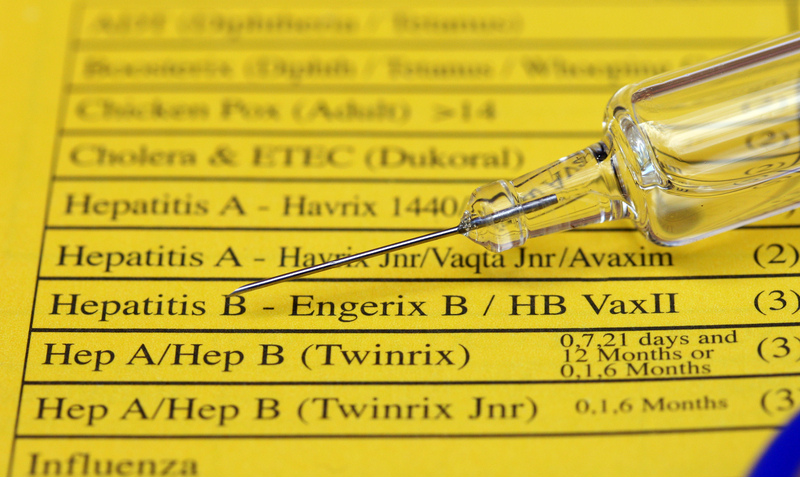
Download and distribute powerful vaccination QI resources for your community.
- Health Champions
Sign up now to support health equity and sustainable health outcomes in your community.
- Cancer Early Detection
MCED tests use a simple blood draw to screen for many kinds of cancer at once.
- PR
FYHN is a bridge connecting health information providers to BIPOC communities in a trusted environment.
- Medicare
Discover an honest look at our Medicare system.
- Alliance for Representative Clinical Trials
ARC was launched to create a network of community clinicians to diversify and bring clinical trials to communities of color and other communities that have been underrepresented.
- Reducing Patient Risk
The single most important purpose of our healthcare system is to reduce patient risk for an acute event.
- Jessica Wilson
- Subash Kafle
- Jessica Wilson