The foundation of American medical innovation, including breakthroughs like mRNA vaccines and CRISPR technology, is facing a severe threat as proposed federal budget cuts loom over the National Institutes of Health (NIH), according to a new report from the Information Technology and Innovation Foundation (ITIF). The analysis warns that deep funding reductions, coupled with accelerating investment from global competitors, risk ceding U.S. biopharmaceutical leadership, undermining national security, and slowing the pace of life-saving medical discoveries.
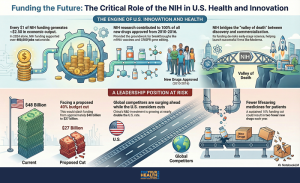
The NIH, established in the early 20th century, is the world’s largest public funder of biomedical research, investing nearly $50 billion annually into its own laboratories and over 2,500 institutions across the United States. This public investment is crucial because it supports foundational, or basic, scientific research—studies on genes, cells, and disease mechanisms—that often lack immediate commercial returns and are thus less appealing to the private sector. Yet, this basic science provides the essential groundwork for future medical advances; for instance, between 2010 and 2016, NIH-funded research contributed biological, chemical, or molecular insights to the development of all 210 new drugs approved by the Food and Drug Administration (FDA). Furthermore, the NIH helps bridge the “valley of death,” the high-risk stage between lab discovery and commercial viability, through programs like the National Center for Advancing Translational Sciences (NCATS) and grants that support biotechnology startups.
Case studies reveal the profound impact of this sustained public funding. The rapid development of mRNA vaccines during the COVID-19 pandemic was enabled by decades of NIH-supported research that began in the late 1980s, culminating in breakthroughs like the pseudouridine substitution in 2005 that made therapeutic use viable. Similarly, the revolutionary CRISPR-Cas9 gene editing technology is rooted in decades of federally funded basic research into bacterial immune systems, demonstrating how long-term public commitment fuels transformative health technologies. This investment has tangible effects on patient outcomes, exemplified by targeted cancer therapies like Gleevec for chronic myeloid leukemia (CML) and Herceptin for HER2-driven breast cancer, which transformed once-fatal diseases into manageable conditions after their underlying molecular targets were identified through NIH-supported research.
Beyond specific diseases, sustained investment is critical for addressing health equity and preparing for future crises. For instance, the proposed FY2026 budget would reduce NIH funding by a staggering 40 percent—from approximately $48 billion in 2025 to about $27 billion in 2026—a cut that would specifically eliminate entire institutes, including the National Institute on Minority Health and Health Disparities and the National Institute of Nursing Research. However, programs like the All of Us Research Program are attempting to mitigate long-standing disparities by building one of the world’s most diverse genetic data repositories, intentionally including participants historically underrepresented in biomedical research. Funding also supports emerging frontiers such as Artificial Intelligence (AI) in drug development, where NIH initiatives like the Bridge to Artificial Intelligence (Bridge2AI) program are creating the high-quality datasets necessary to power the next generation of representative and reliable models. Furthermore, NIH initiatives like the ReVAMPP network proactively advance countermeasures against high-risk virus families to strengthen pandemic preparedness, while ongoing support for early-stage discovery helps combat the escalating global health security challenge of antimicrobial resistance (AMR).
This domestic contraction comes at a time when global competition in the life sciences is intensifying rapidly. While the U.S. weighs steep cuts—which have already led to the reported cancellation of over 2,100 grants worth approximately $9.5 billion, prompting universities to pause hiring and delay clinical trials—strategic rivals are dramatically increasing investment. China, for example, has developed a comprehensive national strategy to bolster its biopharmaceutical capacity, increasing R&D investment by 8.9 percent annually between 2019 and 2023, nearly matching U.S. total R&D spending in 2023. Similarly, the European Union launched Horizon Europe with a budget exceeding €95 billion to support collaborative health and research. Experts warn that if U.S. science budgets are cut, China could soon surpass the United States in R&D spending, posing a direct threat to U.S. leadership in high-value markets and potentially leaving the U.S. reactive in a future global health crisis. Already, prominent scientists have warned that budget cuts could jeopardize future breakthroughs, noting that reduced opportunities may prompt top U.S.-based scientists to move their labs abroad, creating a “brain drain” that weakens America’s capacity for innovation.
Sustained public investment in the NIH is not simply a budgetary matter but a strategic pillar of U.S. strength. Every dollar invested by the NIH generates roughly $2.50 in short-term economic returns and stimulates additional long-term private-sector R&D investment. As global competitors funnel massive public funds into biopharmaceutical innovation, maintaining robust NIH funding is essential to preserve America’s biopharmaceutical leadership, protect national security, and sustain long-term economic prosperity.
The original paper, “How NIH-Funded Science Supports US Biopharmaceutical Innovation,” was authored by Sandra Barbosu and Sarina Fereydooni and published by the Information Technology and Innovation Foundation (ITIF) on December 15, 2025. It can be found on the ITIF website.
Stay Informed. Stay Empowered.
Trending Topics
Features
- Drive Toolkit
Download and distribute powerful vaccination QI resources for your community.
- Health Champions
Sign up now to support health equity and sustainable health outcomes in your community.
- Cancer Early Detection
MCED tests use a simple blood draw to screen for many kinds of cancer at once.
- PR
FYHN is a bridge connecting health information providers to BIPOC communities in a trusted environment.
- Medicare
Discover an honest look at our Medicare system.
- Alliance for Representative Clinical Trials
ARC was launched to create a network of community clinicians to diversify and bring clinical trials to communities of color and other communities that have been underrepresented.
- Reducing Patient Risk
The single most important purpose of our healthcare system is to reduce patient risk for an acute event.
- Subash Kafle
- Jessica Wilson
- Jessica Wilson