- By Jessica Wilson

As the United States moves deeper into the 2025–26 respiratory virus season, public health officials are raising concern about persistently low rates of COVID-19 booster and influenza vaccination uptake even as both viruses continue to circulate and cause serious illness. Federal data and independent surveys show that a majority of adults have not received the updated COVID-19 vaccine or a seasonal flu shot, leaving large segments of the population vulnerable to preventable disease, hospitalization, and death.
According to recent data from the Centers for Disease Control and Prevention and national surveys, only a minority of U.S. adults have received the updated COVID-19 vaccine for the current season. One survey published by the Pew Research Center found that just 27 percent of adults reported having gotten the updated COVID vaccine since it became available, while 42 percent reported receiving a flu shot. More than half of adults (53 percent) said they had received neither vaccine.
CDC’s own behavioral and social drivers dashboard shows low coverage levels as of April 2025, with about one in five adults vaccinated against COVID-19 for the season and fewer than half receiving a flu vaccine. Coverage was highest among older adults, but remained far below optimal levels for broad community protection. CDC These numbers represent a significant drop from earlier phases of the pandemic when comprehensive vaccination campaigns drove substantially higher uptake.
The agency continues to recommend updated COVID-19 and influenza vaccines for nearly everyone ages 6 months and older to protect against severe outcomes, including hospitalization and death. CDC’s guidance emphasizes that the virus that causes COVID-19, SARS-CoV-2, is constantly evolving and that immunity from prior vaccination or infection declines over time, making annual or periodic boosts a key strategy to restore protection against circulating variants. CDC
Despite these recommendations, uptake remains stubbornly low, in part because of public confusion, shifting guidance, and reduced sense of urgency about respiratory viruses now that severe COVID-19 disease has become less common than during earlier waves. In some regions, public health officials have observed booster rates this year that are roughly half of what they were at the same point in the previous year.
The consequences of low vaccination rates extend beyond missed opportunities to prevent mild illness. COVID-19 continues to cause hospitalizations and deaths. Federal hospitalization surveillance data show that COVID-19 hospitalizations have remained substantially higher than those from influenza over recent seasons, underscoring that the virus still poses a significant health burden. U.S. Food and Drug Administration At the same time, influenza hospitalizations and deaths also remain a serious annual public health challenge, with recent years seeing tens of thousands of flu-related deaths in the United States.
Experts stress that vaccination not only reduces the risk of severe outcomes from acute infection but may also lower the likelihood of lingering complications such as Long COVID, a condition marked by persistent symptoms lasting weeks or months after infection. Updated vaccines are designed to target the most common circulating strains of SARS-CoV-2 and influenza viruses, offering a critical tool for maintaining population immunity and mitigating strain on healthcare systems.
Health equity concerns deepen the urgency of improving uptake. Historical and ongoing disparities in vaccination coverage by race, ethnicity, and socioeconomic status mean that communities of color and underserved populations often bear a disproportionate share of severe disease and mortality from respiratory viruses. Lower rates of vaccine access and acceptance in these communities have been documented in past seasons and underscore the need for targeted outreach and culturally competent communication to ensure equitable protection.
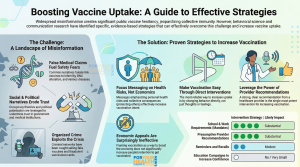
Public health organizations are calling for renewed efforts to address barriers to vaccination, including expanding clinic access in underserved neighborhoods, engaging trusted local health providers in education campaigns, and simplifying messaging about who should get vaccinated and when. The public health trade group AHIP announced that major insurers will continue coverage of both COVID-19 and flu vaccines through the end of 2026, removing a potential cost barrier for many individuals.
Despite the complexity of the current vaccination landscape, the core message from health authorities remains clear: COVID-19 and influenza continue to pose real health risks, and vaccines remain the most effective way to prevent severe illness. As the 2025–26 season progresses, medical professionals urge eligible individuals to speak with their healthcare providers about receiving updated COVID-19 and flu vaccines to protect themselves and their communities.
As the respiratory virus season intensifies, the choice to get boosted becomes more than an individual decision—it is a collective measure to reduce strain on hospitals, protect vulnerable populations, and curb preventable illness. In communities where vaccination rates lag, the coming months will test efforts to close immunity gaps and safeguard public health before the next wave of infections arrives.
Stay Informed. Stay Empowered.
Trending Topics
Features
- Drive Toolkit
Download and distribute powerful vaccination QI resources for your community.
- Health Champions
Sign up now to support health equity and sustainable health outcomes in your community.
- Cancer Early Detection
MCED tests use a simple blood draw to screen for many kinds of cancer at once.
- PR
FYHN is a bridge connecting health information providers to BIPOC communities in a trusted environment.
- Medicare
Discover an honest look at our Medicare system.
- Alliance for Representative Clinical Trials
ARC was launched to create a network of community clinicians to diversify and bring clinical trials to communities of color and other communities that have been underrepresented.
- Reducing Patient Risk
The single most important purpose of our healthcare system is to reduce patient risk for an acute event.
- Jessica Wilson
- Victor Mejia
- Subash Kafle